Pediatric Obstructive Sleep Apnea Case Study
Margaret-Ann Carno PhD, CPNP, D,ABSM
for the Sleep Education for Pulmonary Fellows and Practitioners,
SRN ATS Committee
Part 1: Case Presentation
You are conducting a follow up visit of a 6 year old African American male who was initially referred to you for “wheezing” both during the day and night, night time cough, what mom describes as unable to catch his breath at night and with exercise, and nightly snoring. During the prior visit you diagnosed the child with “asthma” on the basis of history and physical exam ( wheezing) His other past medication history included eczema. Now on low dose ICS and albuterol prn for 3 weeks, Mom states that wheezing has improved and now does not interfere with physical activity. She is still concerned though about the continued snoring, she thought that it was related to the asthma and would be gone by now.
Questions
- What questions/surveys/questionnaires would be appropriate at this visit?
- How often does snoring occur in asthma treatment?
- Is there a differential diagnosis? Does OSA present as asthma? True asthma/True OSA: related or unrelated?
Case Presentation
Mom states, the snoring is almost nightly but… everyone snores in the household. Two mornings a week the child awakens complaining of a headache. The teacher has reported that while he is doing “fine” in school he just cannot stay still and needs directions repeated. Mom states that she “Does not think that this is an issue as he is just a boy!”
You now look at his chart, Height is 1.182 m, Weight is 24.3Kg the BMI %ile is 89% ( z-score is 1.25), heart rate is 90, respiratory rate is 20, oxygen saturations are 98% and Blood pressure is 90/60.
Physical Exam
- You conduct your physical exam; Breath sounds are equal clear, good aeration and no wheezing is heard. Heart sounds, regular rate, with a physiological split of S2. No clubbing of the finger nail beds are noted, the abdomen is soft, obese, non-distended, non-tender, the palate is in a dependent position and tonsils are enlarged, almost touching the uvula
- Finally the nasal mucosa is redden and swollen but not with a large amount of white mucous. No polyps are seen.
- What are important components of a good sleep physical examination?
- What are risk factors for pediatric obstructive sleep apnea, in general, and this patient in particular?
- What are symptoms of sleep disordered breathing in children?
- What test would you order and how would you explain this to the child and mom? What features in a child study are important, compared to an adult study.
Part II: Diagnostic Testing
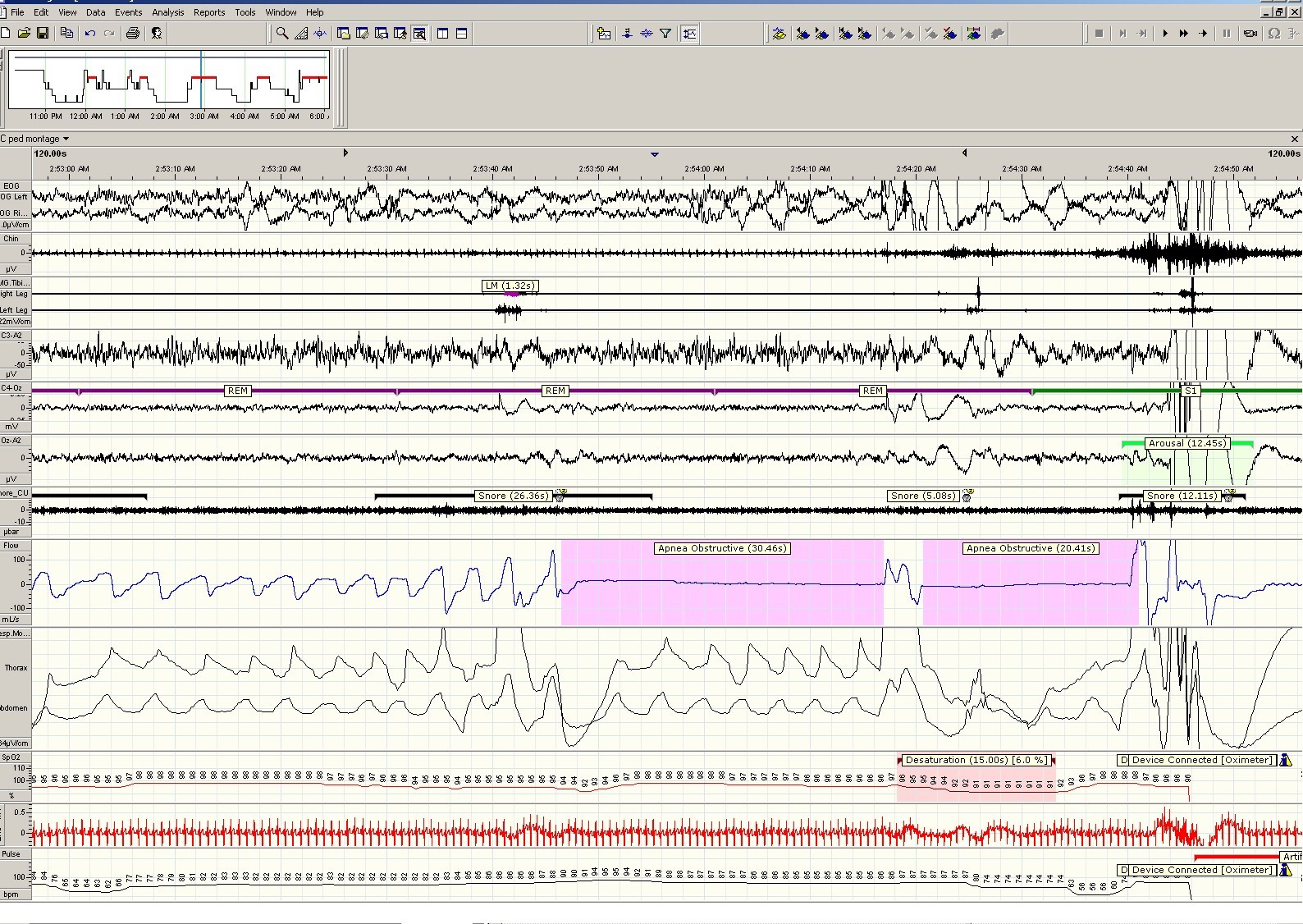
You consider him at high risk for sleep-disordered breathing and request in- lab, attended polysomnography. The sleep study report is as follows:
SLEEP ARCHITECTURE: (frontal, central and occipital EEG, right and left EOG and digastric EMG) fragmentation of sleep stages, increase in arousals, limb movements within normal limits
RESPIRATION: The obstructive apnea-hypopnea index (AHI) was 12.5 per hour of sleep.
OXYHEMOGLOBIN SAT URAT ION: (pulse oximetry with beat by beat sampling) Mean oxyhemoglobin saturation was 95%. Oxyhemoglobin saturation was below 88% for 5 minutes. The SaO2 ranged from 98-84%. The patient was studied on room air.
EtCO2 was within normal range
Questions
- What alternative tests are available to diagnose sleep disordered breathing?
- What are the metrics for norms and for OSA in this age group? What is the difference between overall AHI vs obstructive AHI, or apnea or hypopnea? Is position important?
- What treatment options are available for sleep disordered breathing and what would you recommend for this patient?
Part III: Treatment and more questions to Ponder
Do you make and present treatment options/recommendations based on PSG alone?
Mom asks how her son’s sleep apnea relates to his asthma, eczema and his daytime behavior How would you answer her?
Part III: Treatment
After some discussion with mom she agrees to bring her son to see an ENT doctor for a possible T&A.
- Your office assists in making the appointment for mom. What information is relevant for the referral?
Questions
- Why is T&A first line treatment for children with OSA?
- What are the chances that a T&A will completely cure this child’s OSA?
- Would you repeat the overnight PSG after surgery? Why or Why not?
- Mom and the child returns 12 weeks after the T&A. There were no complications but mom states that the snoring has decreased only a little.
- Why do you think that the snoring and daytime symptoms have not resolved completely?
- What do you do now?
- After talking at length with mom, she agrees to bring the child back for a repeat overnight sleep study
- The results of the study : Obstructive AHI 6 events/hour
- Why did the T&A not completely resolve the OSA?
- What is your next treatment option?
- You order an CPAP titration after the child undergoes a mask fitting session
- Why is it important to make sure that the mask fits the child?
- The child undergoes the CPAP titration study a pressure of 7 CmH2O relieves the child’s OSA
- How do you monitor compliance in a child on CPAP?
- How do you monitor CPAP adherence in children?
Conclusion
SA returns after 3 months of CPAP use and Mom reports improvements in daytime hyperactivity, concentration, and school performance. Weight has not changed.
Compliance download demonstrates 5 hour average use every night with heated humidification. Is this enough or just a start?
Download the Facilitator Guide.
Download case in PowerPoint or PDF.
Please complete the online survey and download your certificate.