Article:
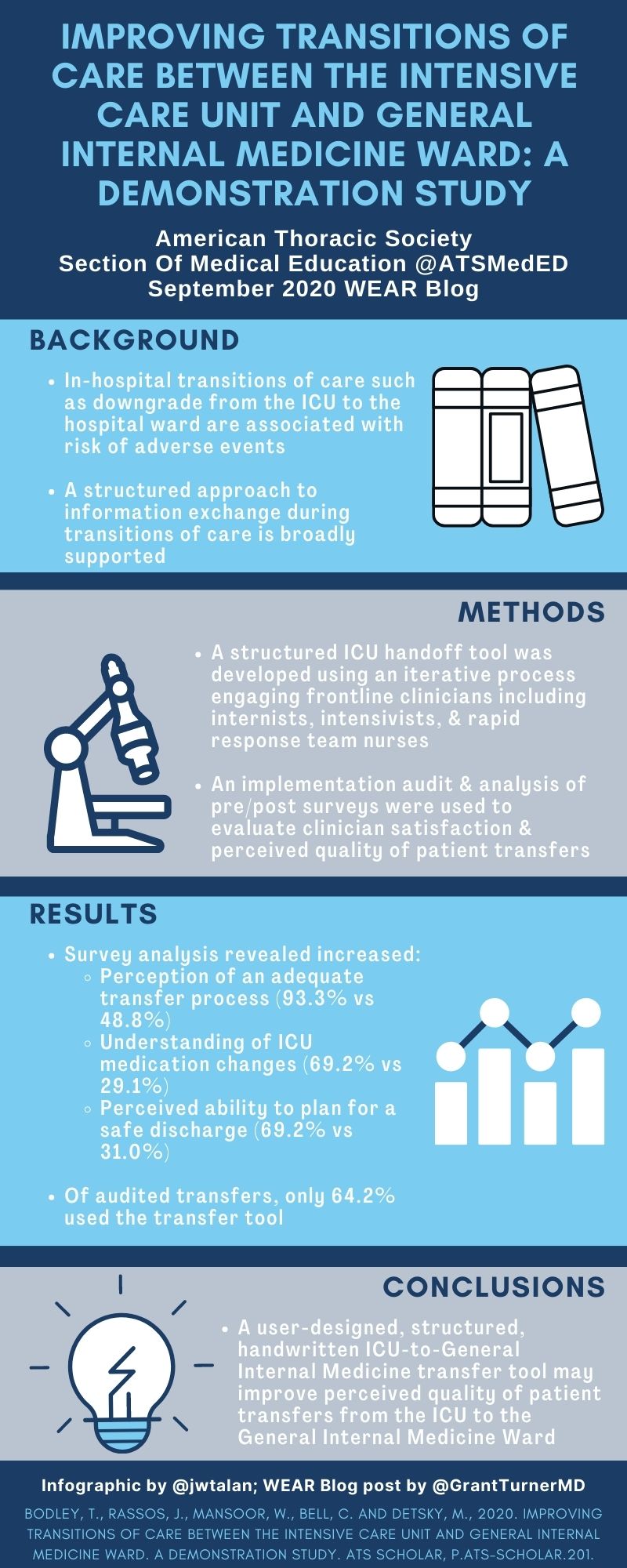
Bodley T, Rassos J, Mansoor W, Bell CM, Detsky ME: Improving Transitions of Care between the Intensive Care Unit and General Internal Medicine Ward. A Demonstration Study. ATS Scholar 2020.
Summary:
Transfers from the Intensive Care Unit (ICU) to the General Internal Medicine (GIM) ward represent time with increased risk for a patient, including medication errors, unclear changes in the treatment plan. They are a frequent cause for dissatisfaction for patients, families, and clinicians. In this study, the authors hypothesized by standardizing the handover between the ICU and GIM team through a handwritten tool would improve not only the transfer process but also clinician engagement and enhance satisfaction. A standardized handover tool was created using stakeholder engagement and usability/comprehensiveness testing. For three months, the instrument was used by the ICU and GIM teams, with pre and post-intervention surveys for evaluation of understanding regarding the patient's hospital course. Clinicians felt that ICU transfers were improved by the use of this tool, with limitations of the use of paper charting at their location, complicating full use of the tool in all situations. For this blog post, Dr. Grant Turner interviewed first author Dr. Thomas Bodley.
Interview:
GT: In your study, you create a tool for effective Intensive Care Unit (ICU) to General Internal Medicine (GIM) handovers to improve overall care for the patient; in the study, you mention only 59.4% of GIM Physicians noted an excellent understanding of the patient's reason for admission and hospital course which improved to 92.3% after the intervention. From your experience, was there a specific component of the handover tool that was most useful for participants, or was the creation of the tool in its entirety the key to its success?
TB: I'm glad you ask, because there are certain elements of the transfer tool that worked well, and others that did not. Understanding the reason for hospital admission and course in hospital are critical to developing a shared patient care model between the sending and receiving provider. These elements were mostly captured in the tool sections "primary and secondary diagnosis" - which were frequently completed sections during our tool audits. Since diagnosis is an evolving care process, having the critical care team clearly identify and synthesize their team's opinion and action plan at the time of ward transfer is important for the accepting team. I suspect similar information is conveyed during a verbal handover (which also occurs with each ICU transfer), though our qualitative analysis shows this isn't always the case. Since verbal handover occurs between one sending and one receiving provider, our tool has the added advantage of a permanent document that can be referenced by multiple clinicians in the days following ICU to ward transfer.
One area that was not well completed was the home medications section. There are multiple potential reasons for this; most importantly is that a "best possible medication history" or "BPMH" is completed at the time of admission to hospital by our pharmacy team. In retrospect, the home medication section was therefore redundant. Future tool iterations could omit this section and simply attach the BPMH to save time for front line clinicians. That said, home medications are a critical element of ICU to ward handovers since we know that neglecting to restart important home medications after an ICU admission is a common error.
GT: You note that a limitation of your study is the use of paper charts and the handwritten nature of the handover, potentially limiting the ability of allied health care participants to participate in the transfer process. Knowing that this continues to be a problem in many ICUs, do you have ideas of how information from other specialties (Pharmacy, Physical Therapy/Occupational Therapy, Social Work, etc) can be included in future versions of a standardized handover tool?
TB: Our intention through stakeholder engagement was to make our tool multidisciplinary both in terms of content and during tool completion. For anyone embarking on an ICU to ward transfer project, I strongly recommend spending extra time working through tool development while paying close attention to the needs of your local environment. In these types of quality interventions, context really is critical. Our Figure 1 provides a sound starting point for anyone looking to develop their own institutional transfer tool.
To answer your question, there are a few elements of ICU to ward transfers that make multidisciplinary contribution to a handwritten transfer tool challenging. For one, transfer timing is often unpredictable. Sometimes patients are transferred after hours, or even over night when beds are emergently needed. In these situations, the medical team needs to get transfer documentation done quickly, and don't have time to engage all the appropriate clinicians. I think the ideal handover tool would be integrated with the electronic health record, and automatically updated in real time to avoid too much manual data entry. Unfortunately, this is a long way off.
I'd also mention that options to engage the multidisciplinary team in handovers go beyond tool development/completion. For example, I think future studies looking at ways to execute ICU to ward transfer in person with all relevant stakeholders at the patient's bedside (similar to multidisciplinary rounds in the ICU - but also engaging the ward team) could be explored.
GT: After the intervention period, are you still using this handover tool or made improvements as you suggested in your article? How has the continued response been to the tool?
TB: After our intervention window we realized that some elements of the transfer tool were overly onerous to complete. This was especially true of the medications sections, which were poorly completed in our tool completion audit as well. As a result, we transitioned from having the transfer document be "required" to making it a suggestion that could also be used as a template rather than a structured form. The process of developing, implementing, and evaluating our transfer tool was a learning journey for our ICU team and I believe it has resulted in a sustained improvement in our ICU to ward transfer process. That being said, future studies at our institution and others should focus on patient important outcome measures - such as medication errors following ICU to ward transfer. Such outcome measures would give us a better idea of whether our interventions are really reaching the patient.
GT: You mention in your study that implementation of handover tools are meant to decrease adverse events, especially those related to transfer between physician teams. Were you able to see a difference in patient safety events at your hospital during the intervention period associated with the use of your handover tool?
TB: This is such an important point, and frequently a challenge in handover studies. Future work needs to focus on patient important outcome measures. We focused on a surrogate or process measure, which was clinician (both nursing and MD) satisfaction and self-reported efficiency of the transfer process. While these are important to clinicians, they don't necessarily reach the patient. Potential outcome measures for future ICU to ward transfer studies could include medication errors after transfer (because they are common) and major adverse events (such as ward cardiac arrest) since they are particularly harmful to patients. I would also point out that engaging patients and their families as important stakeholders should also be considered. Surveys of patient and caregiver satisfaction is another patient centered outcome to consider in this type of work.
Blog post author
Dr. Grant Turner is a fellow in Pulmonary & Critical Care at the University of Nebraska Medical Center in Omaha, Nebraska and currently applying for Lung Transplant Fellowship for 2021-2022. He completed his internal medicine training at Thomas Jefferson University in Philadelphia, Pennsylvania. His academic interests include lung transplant, medical education, patient safety and quality, and LGBTQ+ inclusive subspecialty medical care.
Twitter: @GrantTurnerMD

Article authors
Dr. Thomas Bodley is a Clinical Associate with the Department of Critical Care at Sunnybrook Health Sciences Center in Toronto, Ontario, and a graduate student at the Institute for Health Policy Management and Evaluation at the University of Toronto. Dr. Bodley's research interests include quality improvement and quality assurance in adult critical care. His work focuses on enhancing the use of evidence based practices in mechanically ventilated patients, organizational factors influencing quality improvement initiatives, and provider communication during handover and ICU to ward transfer.
Twitter: @TomBodley